Since Wittich’s first publication in 1941 reporting the successful treatment of allergy in a dog with ASIT (Specific Allergen Immunotherapy), many advances have been made. While human studies are numerous and widely document the efficacy of ASIT in various allergic diseases, particularly allergic rhinitis and asthma, data concerning CAD remain, paradoxically, fragmented.
State of knowledge on canine ASIT
While in humans, some question the usefulness of ASIT in human atopic dermatitis, this controversy has apparently never emerged in veterinary medicine, probably due to encouraging early reports concerning CAD. The absence of controversy in veterinary medicine could also be linked to factors such as the limited number of rigorous clinical studies conducted in dogs, the complexity of evaluating the efficacy of ASIT in the context of CAD, and the variability of therapeutic protocols used across different studies. These factors make direct comparison of results difficult, thus limiting overall conclusions on the efficacy of canine ASIT.
Studies, including a placebo-controlled, blinded study of 51 dogs, have shown response rates (generally defined as the proportion of dogs showing at least 50% improvement in clinical signs) of around 60 to 70%. However, it is crucial to note that, even in positive cases, a significant percentage of dogs (up to 65% in one study) required complementary medication, questioning owners’ ability to objectively judge the efficacy of ASIT. Current guidelines for the treatment of CAD qualify the quality of published evidence regarding the efficacy of ASIT as “limited.” This limitation of evidence is due to several factors, including the small size of many studies, the lack of standardization of protocols, and the difficulty of obtaining objective measures of ASIT efficacy in dogs. It is important to emphasize that the evaluation of ASIT efficacy often relies on subjective owner assessments, which can introduce bias into the results. More objective evaluation methods, such as the use of biomarkers or validated clinical scores, are needed to improve the quality of available evidence.
The interpretation of canine ASIT study results is often complicated by the variability of protocols used. Differences in dosage, allergenic extract composition, injection frequency, concomitant treatments, and outcome evaluation methods make direct comparison of results obtained in different studies difficult. The heterogeneity of dog populations included in studies is another complicating factor. Variability in breeds, ages, CAD severities, and medical histories of dogs can influence ASIT response, making result analysis more complex. To improve data interpretation, future studies should focus on standardizing protocols, homogenizing study populations, and using more objective efficacy measures.
Comparison with human ASIT: Although ASIT is used to treat various allergies in humans, the efficacy and mechanisms of action are not always fully understood, and vary depending on the type of allergy and the individual. There is controversy regarding the usefulness of ASIT in human atopic dermatitis, with some studies questioning its efficacy, while others show positive results. This nuance reflects the complexity of individual immune responses and the heterogeneity of atopic dermatitis. Comparison with human ASIT allows for the identification of research avenues for canine ASIT, but it is important to qualify these comparisons due to physiological and immunological differences between species.
Mechanisms of action: the known and the unknown
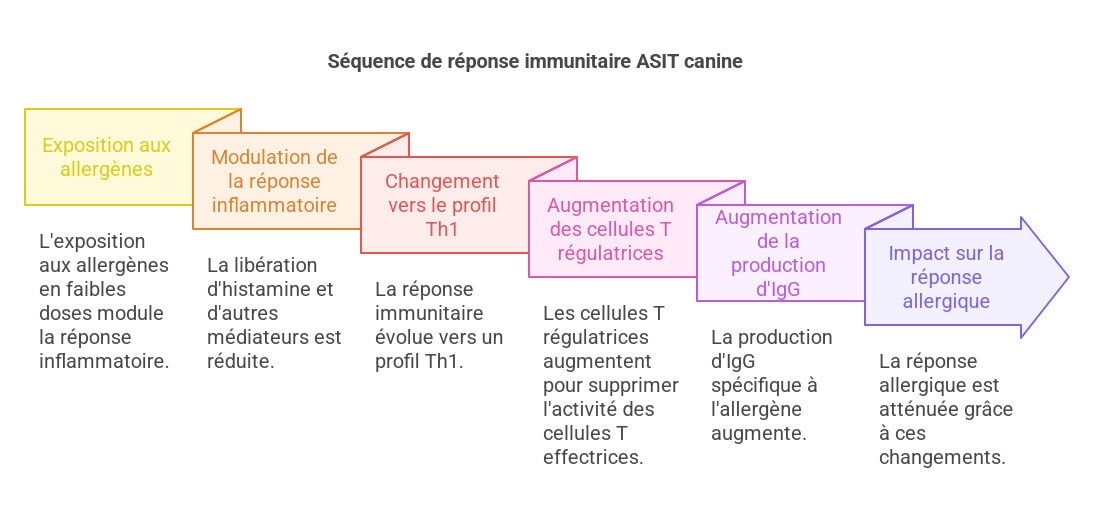
The precise mechanism of action of canine ASIT remains incompletely elucidated. Nevertheless, a parallel with human mechanisms is plausible. In humans, an initial reduction in effector cell activity (eosinophils, basophils, mast cells) is observed, followed by a long-term immunological shift from a Th2 (helper 2) cell response to a Th1 (helper 1) cell response and the development of immunological tolerance. This complex and multifactorial process involves different stages and cell populations.
- Initial phase: Exposure to allergens at low doses causes a modulation of the immediate inflammatory response. This results in a reduction in the release of histamine and other inflammatory mediators by mast cells and basophils, which reduces immediate allergy symptoms. Mast cell degranulation, a key process in the immediate allergic response, is inhibited or attenuated.
- Late phase: The immune response gradually shifts towards a Th1 profile, with an increase in T helper 1 lymphocytes that produce pro-inflammatory cytokines such as interferon-gamma (IFN-γ) and a decrease in T helper 2 lymphocytes and associated cytokines (IL-4, IL-5, IL-13). This Th1/Th2 switch contributes to the regulation of the long-term inflammatory response.
- Role of regulatory T cells (Treg): Treg cells, with markers like FOXP3, play a crucial role in the acquired immune tolerance through ASIT. These cells suppress the activity of effector T lymphocytes, contributing to the calming of the allergic inflammatory reaction. The increase in the number and activity of Treg cells is correlated with a better response to ASIT.
- IgG production: The production of immunoglobulin G (IgG), particularly IgG4, specific to the allergen increases after prolonged treatment. These blocking IgG antibodies could reduce IgE binding to allergens, thereby decreasing their ability to trigger an inflammatory response. However, studies remain uncertain about the actual impact of IgG on reducing the allergic response.
These changes are accompanied by an increase in cytokines such as transforming growth factor beta (TGFβ) and interleukin (IL)-10, anti-inflammatory cytokines playing a role in maintaining immune tolerance. This results in an increase in allergen-specific immunoglobulins (IgG), particularly IgG4, and, with prolonged treatment, a decrease in allergen-specific IgE. In dogs, although knowledge is less extensive, a shift towards a Th1 response, an increase in IgG levels, the appearance of more Treg cells, and increases in IL-10 levels have all been demonstrated, thus establishing parallels with human ASIT. However, studies in dogs are less numerous and less in-depth than in humans, and the exploration of canine ASIT mechanisms of action requires additional research for a more complete understanding. The use of animal models (mice, for example) can help elucidate some mechanisms, but extrapolation to the canine species must be done with caution.
Sublingual administration involves an additional effect through oromucosal dendritic cells. In humans, these cells play an important role in inducing oral tolerance, an immunological process by which the immune system is programmed not to react to substances introduced into the mouth (e.g., food). The precise role of these cells in canine ASIT still needs to be explored.
Current approaches to canine ASIT: efficacy and areas for improvement
Current ASIT approaches for CAD rely on two main administration routes: subcutaneous (SCIT) and sublingual (SLIT). SCIT, practiced for decades, uses phenol-preserved aqueous allergenic extracts in North America and alum-precipitated allergenic extracts in Europe. The use of aluminum-based adjuvants, despite the advantage of less frequent injections, raises growing concerns about their potential long-term side effects, linked to chronic aluminum exposure. In-depth studies on the long-term toxicity of aluminum are needed to fully evaluate the implications of its use in vaccines and allergy treatments. Alternatives to aluminum-based adjuvants are currently being investigated, including more biocompatible and less toxic adjuvants.
SLIT, more common in humans, appeared more recently in veterinary medicine and is subject to controversy in humans regarding the reliability of many older studies with highly variable protocols. Recent analyses and positions from the World Allergy Organization conclude its efficacy and a favorable safety profile compared to SCIT. However, data on canine SLIT are still limited and require additional studies to validate its efficacy and safety in this species. Studies conducted in humans suggest that SLIT could be a more practical and safer approach than SCIT. However, the variability of protocols used in human studies makes it difficult to determine optimal protocols for canine SLIT, requiring future studies for validation of its use in dogs. Similarly, comparative studies between SCIT and SLIT in CAD are essential to evaluate their relative efficacy and the benefits and drawbacks of each method.
Important considerations regarding the quality of the extracts used affect efficacy. Allergen extracts for veterinary use were licensed by the United States Department of Agriculture (USDA) decades ago, based on criteria of safety, purity, sterility, and manufacturing consistency, not on rigorous long-term efficacy studies. This situation highlights the need for new regulations and stricter standards to ensure the quality and efficacy of allergenic extracts used in veterinary medicine.
The scientific literature concerning canine ASIT suffers from a lack of standardization of protocols, with great variability in dosing regimens, allergenic extracts, their composition and potency between manufacturers, administration schedules, concomitant treatments, and extract mixing methods. This lack of standardization limits the comparability of studies and the interpretation of results. The absence of standardized protocols makes it difficult to evaluate the actual efficacy of ASIT and to determine the optimal parameters for CAD treatment.
Details on the different approaches:
- SCIT (Subcutaneous): The allergen is injected under the skin. Several approaches exist, with a gradual increase in doses (induction) and a long-term maintenance schedule. Extracts can be aqueous (North America) or alum-precipitated (Europe) for slower release. The use of alum raises questions about the long-term toxicity of aluminum, requiring studies and a risk-benefit assessment.
- SLIT (Sublingual): The allergen is administered under the tongue, a less invasive approach potentially better for owner compliance. However, more studies and better standardization are needed for its clinical calibration in veterinary practice.
- RIT (Rush Immunotherapy): Rapid administration of increasing allergen doses over a short period, requiring close monitoring. Increased risks of adverse effects exist, but it can be more practical for some dogs.
Improving the standardization of canine ASIT
Establishing the main allergenic epitopes in dogs, particularly for common allergens, would allow for standardization of extracts, uniform dosing, production of recombinant allergens, and the use of peptide immunotherapy. Identifying major allergenic epitopes in dogs allows for the creation of more specific and purified extracts. These standardized extracts allow for better reproducibility of results between different studies, thus improving data reliability. Furthermore, knowledge of epitopes allows for the development of recombinant allergens, synthesized in the laboratory, which allows for the production of purer and more homogeneous allergen preparations.
The allergen dosage is fundamental. In humans, the dose and injection interval affect efficacy. These parameters have not been sufficiently studied in dogs. Dose-response studies are crucial to determine the optimal allergen dose that maximizes efficacy while minimizing adverse effects. Identifying predictive biomarkers of ASIT response could also allow for personalized treatment based on the dog’s individual response.
Similarly, rush immunotherapy (RIT) offers advantages in terms of the number of home injections but also increased safety risks and higher cost due to necessary hospitalization. Rush immunotherapy (RIT) is an approach that allows allergen doses to be administered more quickly. This can reduce treatment duration and improve owner compliance, but increases the risk of adverse effects. To optimize RIT use, it is necessary to better document the safety and efficacy of this method, and possibly design less intensive protocols to reduce risks while preserving efficacy. Studies comparing RIT with conventional immunotherapy are needed.
Optimization of canine ASIT protocols
Standardizing canine ASIT protocols represents a major challenge. The optimal number of extracts in a mixture remains to be defined, as does how to manage extracts containing proteases, such as molds. Protocol standardization requires a multifactorial approach. It is necessary to define the optimal treatment parameters, including:
- Number and type of allergens: Determine the number of allergens to include in the mixture. Studies suggest that a single dominant allergen may be sufficient, even in cases of polysensitization, although this approach is less common in North America than in Europe.
- Protease management: Molds contain proteases that can degrade other allergens. This can compromise the effectiveness of the allergen mixture. Managing this problem requires further study.
- Allergen selection methods: Use intradermal tests, serological tests, or a combination of both. The limitations of each method must be taken into account. Additional research is needed to determine the optimal method of allergen selection for canine ASIT.
- Allergen mixture formulation: More studies are needed to determine the best approach, which will improve the reproducibility of studies.
Official guidelines recommend not mixing mold and pollen extracts in the same vial due to the degradation of pollen allergens by fungal proteases during storage. Similar, but less conclusive, data exist for dogs. These recommendations highlight the need for a better understanding of the interactions between different allergens in the mixture. It is important to consider potential enzymatic degradations at the level of the different components of the mixture and thus to determine the optimal formulation to ensure long-term efficacy.
Biomarkers of therapeutic success and new approaches
The use of biomarkers for objective evaluation of canine ASIT success is essential to improve clinical studies, address the lack of reproducible data, and overcome the significant placebo effect. Although increases in total serum IgG1 concentrations, specific IgG responses to house dust mite immunotherapy, and changes in different levels of Treg cells have been observed in dogs, these findings have not been sufficiently investigated to serve as a means of objective and rapid evaluation of ASIT success. The identification of reliable biomarkers would allow for a better evaluation of treatment efficacy and a better prediction of individual response to ASIT.
Potential biomarkers to explore include:
- Serum IgG concentrations (especially IgG4): An increase in allergen-specific IgGs could correspond to clinical improvement. The measurement of IgG4 is particularly promising, as this IgG subclass is particularly linked to the induction of tolerance.
- Regulatory T cells (Treg): The number and activity of Treg cells are key indicators of immune tolerance. Measuring circulating or tissue Tregs could be useful for monitoring ASIT response.
- Anti-inflammatory cytokines (IL-10, TGF-β): An increase in these cytokines could indicate a decrease in allergic inflammation.
- Effector cell activity (eosinophils, basophils, mast cells): A decrease in activity could be correlated with a better clinical response.
- Objective measurements of pruritus: For example, the use of accelerometers to quantify scratching activity.
The use of combined biomarkers could provide a more complete picture of the ASIT response, thus improving the interpretation of clinical study results.
New therapeutic approaches
The development of modified allergen preparations (allergoids, recombinant allergens or peptides) and the improvement of allergen efficacy via adjuvants (IL-10 inducers, encapsulation in virus-like particles (VLPs) or in SLIT cases, mucoadhesive polymers) represent promising avenues for progress. These modified preparations offer several advantages:
- Allergoids: Chemically modified allergens to reduce their ability to trigger an immediate allergic reaction, while retaining their immunogenic capacity. This would reduce the risk of adverse effects.
- Recombinant allergens: Allergens produced in the laboratory, offering superior purity and homogeneity to natural extracts.
- Allergenic peptides: Small fragments of allergens containing T-cell specific epitopes, minimizing the risk of anaphylaxis.
Adding immunomodulators (CpG oligodeoxynucleotides, specific monoclonal antibodies) could direct the immune response towards specific tolerance while moderating the “cytokine storm” in active inflammation. These immunomodulators allow manipulation of the immune response, promoting anti-inflammatory responses and immune tolerance. CpG ODNs stimulate innate immunity by activating dendritic cells and NK cells, and monoclonal antibodies can target specific pro-inflammatory cytokines.
Studies on alternative administration routes (epicardial or intralymphatic immunotherapy) are proving promising. Epicardial immunotherapy applied topically to the skin could induce local and systemic tolerance to allergens. Intralymphatic immunotherapy, consisting of injecting the allergen directly into the lymph nodes, could optimize contact with immune cells involved in the development of tolerance. Although studies exist on intralymphatic immunotherapy in dogs, further research is needed to determine optimal protocols and to evaluate its long-term efficacy and safety. Furthermore, intralymphatic immunotherapy could be less restrictive for the owner compared to conventional subcutaneous immunotherapy, which would improve therapeutic compliance.
Furthermore, advances in immunotherapy for human food allergies, particularly the use of molecular diagnostics and alternative administration methods, could inspire innovative approaches for CAD. Optimizing the diagnosis of food allergies in dogs is an important research avenue. More precise molecular diagnostic methods could identify the specific food allergens responsible for reactions. New administration methods, such as oral treatments, could improve dogs’ tolerance to allergenic proteins. Advances made in humans could be a source of inspiration for adapting these approaches in the context of CAD.
ASIT versus new treatments
Finally, it is important to remember that, in the face of the efficacy of new treatments such as cyclosporine, oclacitinib, or anti-IL-31 monoclonal antibodies, the place of ASIT in the multimodal treatment of canine allergies requires constant consideration. Nevertheless, ASIT remains the only therapy capable of modifying or reversing at least part of the pathogenesis and offering the prospect of a definitive cure. It is therefore essential that ASIT be considered not as a last-resort treatment, but as a therapeutic option to be considered as a first-line treatment. ASIT can be a first-line therapeutic option, especially in dogs that do not respond well to conventional drug treatments, or in those that experience adverse effects from these medications. Combining ASIT with other treatments can improve the overall efficacy of CAD treatment. It is important to consider the safety profile and relative efficacy of the different available treatments.
Comparison with alternative treatments: Cyclosporine, oclacitinib, and anti-IL-31 monoclonal antibodies are effective treatments for relieving CAD symptoms, but they do not modify the disease’s pathogenesis and their long-term administration is necessary. ASIT, on the other hand, targets the root cause of the allergy by modifying the dog’s immune response. Although ASIT may take time to produce an effect, it offers the prospect of a complete cure, as opposed to symptomatic treatments. The combined use of ASIT and symptomatic treatments is a possible approach.
Conclusion and perspectives
In conclusion, although ASIT is a promising therapeutic option for canine atopic dermatitis, its efficacy remains to be formally demonstrated by rigorous and better standardized clinical studies. The mechanisms of action remain enigmatic, and additional avenues of investigation are needed. More numerous and rigorous studies are essential to fill the current gaps in knowledge. In particular, it is necessary to better understand the mechanisms of action, determine the optimal treatment parameters, and identify reliable biomarkers to evaluate efficacy and predict response.
Future studies should focus on:
- Precise identification of canine allergens: Development of more accurate and standardized diagnostic tests to identify the allergens involved.
- Optimization of administration protocols: Standardization of protocols and comparison of different administration methods (SCIT, SLIT, RIT, ILIT). Rigorous comparative studies are needed.
- Identification of predictive biomarkers for therapeutic success: Determine markers that can predict treatment response before administration. This will allow for personalized treatment.
- Exploration of modified allergenic preparations: Testing recombinant allergens, peptides, and allergoids. These purer formulations could improve safety and efficacy.
- Immunomodulatory strategies: Testing the use of immunomodulators to influence the immune response and optimize tolerance.
- Long-term studies: Evaluating the long-term effects of different protocols, to better understand the durability of treatment efficacy.
ASIT could thus become a first-line treatment in the management of CAD, instead of remaining confined to a second-line option. The improvement of protocols, standardization, and the development of new diagnostic and therapeutic tools will make ASIT a tool of choice in the treatment of canine atopic dermatitis.
FAQs
Q1: What are the limitations of intradermal and serological tests for diagnosing CAD?
Intradermal tests (IDT) and serological tests for the determination of allergen-specific IgE (ASIS) have limitations. IDTs do not measure the sensitivity of all allergic pathways, and falsely positive reactions in non-allergic dogs have been described. False positive reactions are more common at higher concentrations, and positive results may be linked to non-specific IgE sensitivity (cross-reactions with other allergens). ASIS only measure circulating allergen-specific IgE and do not account for other allergic pathways, and falsely positive reactions have also been observed. Furthermore, both tests lack standardization, and false positive and false negative results are possible. Sensitivity can vary from one laboratory to another.
It is estimated that between 10 and 30% of dogs with clinically confirmed CAD may present a negative IDT, due to various factors such as technique, allergen concentration, drug interference, intrinsic host factors, or inaccurate allergen selection. The limitations of intradermal tests also include the need for specific dog preparation (shaving, etc.), the risk of local reactions, and the subjectivity of result interpretation. Serological tests (ASIS) avoid these drawbacks but have limitations in terms of sensitivity and specificity; positive reactions can be observed in non-allergic dogs.
Ultimately, these allergological tests are only useful for determining the allergens to include in desensitization, and in no case for the diagnosis of canine atopic dermatitis.
Q2: How to choose allergens for an ASIT protocol?
The choice of allergens for an ASIT protocol should be based on the animal’s clinical history, in association with positive reactions to intradermal or serological tests. However, one should not rely solely on tests, as positive reactions can be observed in healthy dogs, and reactions do not necessarily reflect clinical hypersensitivity. Careful interpretation of the clinical history and correlation with test results allows for the identification of relevant allergens for the establishment of the therapeutic protocol. Provocation tests could be considered in some cases.
Q3: What are the advantages and disadvantages of rush immunotherapy (RIT)?
Rush immunotherapy (RIT) reduces the induction period compared to conventional immunotherapy. In dogs, RIT is well tolerated, with major adverse effects being rare, and it is mainly associated with pruritus. However, it requires hospitalized clinical monitoring, and this type of approach carries greater safety risks, in addition to increased cost. RIT can be considered in dogs where the risk of anaphylaxis is low, allowing time to be gained if tolerance is good. Optimization of protocols will require further evaluation to identify optimal safety parameters and avoid adverse reactions. Comparison between classical RIT is necessary.
Q4: What are the new research avenues concerning canine ASIT?
Several research areas deserve to be explored: the use of modified allergenic preparations (allergoids, recombinant allergens, peptides), the development of new adjuvants to improve treatment efficacy and safety, the identification of biomarkers of therapeutic success, and the standardization of protocols. The exploration of innovative administration techniques, such as intralymphatic, epicutaneous, or oral immunotherapy, is also promising. Research on canine ASIT is a constantly developing field, and new research avenues are always being explored. A standardization effort to improve the reliability of studies is essential.
Q5: Are there any drug interactions to consider before performing skin tests?
Drug administration can influence IDT results. Certain medications, such as antihistamines, glucocorticoids, cyclosporine, and tricyclic antidepressants, can interfere with IDTs. A withdrawal period for certain medications may be necessary before performing an IDT. Potential drug interactions must be taken into account before starting treatment. The effect of medications must be considered before performing tests. A discussion with the veterinarian is essential to determine the potential discontinuation of some medications before testing. Potential interaction with the medication used in the treatment of the disease must be considered.
References
Hensel P, Santoro D, Favrot C, Hill P, Griffin C. Canine atopic dermatitis: detailed guidelines for diagnosis and allergen identification. BMC Veterinary Research 2015; 11:196. DOI: 10.1186/s12917-015-0515-5.
Mueller RS. Update on Allergen Immunotherapy. Vet Clin Small Anim 2019; 49: 1–7. DOI: 10.1016/j.cvsm.2018.08.001.
DeBoer DJ. The future of immunotherapy for canine atopic dermatitis: a review. Vet Dermatol 2017; 28: 25–66. DOI: 10.1111/vde.12416.
Pinto MSN, Gil SJRC, Ramió-Lluch L, et al. Challenging the norm: Epicutaneous immunotherapy for canine atopic dermatitis. Allergy 2023; 78: 255–257. DOI: 10.1111/all.15946.
Related Searches
canine atopic dermatitis treatment, atopic dermatitis, dermatitis, dogs, atopic in dogs, in dogs, atopic dermatitis in, genetic disease, canine atopic dermatitis, animal, treatment, disease, skin, allergy, something, skin barrier, itching, lesions, cat, test, mites, in a dog, desensitization, pollens, pruritus, essential fatty acids, duration, vaccine, life, scheme, allergens, molds, strengthen skin barrier, cad, dermitis, side effects, fatty acids, atopic, owner, diseases, symptoms, management, substances, humans, immune system, fleas, golden retriever, causes, goal, rule, age, jack russel terrier, bites, breeds, health, pathology, charge, allergology, effect, inflammation, barrier, microorganisms, form, shar pei, redness, case, origin, function, flea bites, flare-ups, predisposition, phase, companion